Engineers Tackle Ebola
The current gold standard for detecting the Ebola virus is called polymerase chain reaction (PCR), and within a few hours it can detect from oral swabs if viral RNA is present. But a new procedure called RPA, or recombinase polymerase amplification, can detect the virus within 30 minutes, according to researchers at Germany’s Gottingen University and the German Primate Center.

Moreover, the team of researchers has packaged the test into a portable “suitcase” lab that’s solar powered, so it can be used in remote areas.
In a recent field study in Guinea, in which 928 swab samples were tested, 808 were negative and 120 were positive, and the accuracy was 100 percent, which matches the efficacy of PCR tests. But the team says the RPA method is not only faster; it’s technically simpler. Ebola outbreaks are easier to control when on-site diagnoses can be done as quickly as possible. The kit could also be used to detect other dangerous infectious diseases, including the Dengue virus.
This article first appeared in the December 2015 First Look section of ASEE’s Prism magazine and was written by chief correspondent Thomas K. Grose.
A year earlier, Harvard University researchers announced the development of a rapid, paper-based diagnostic test for the Ebola virus using RT-PCR, or reverse transcription polymerase chain reaction. The process is very accurate and produces no false positives, but it’s rather slow – four hours for results – and expensive: $60 to $200 per test. The method invented by James Collins, a biomedical engineer at Harvard’s Wyss Institute for Biologically Inspired Engineering and a pioneer of synthetic biology, can detect Ebola within 30 minutes using paper strips that cost only 4 to 65 cents to make. He uses a so-called cell free system that mimics a cell’s processes. Collins’s team mixed together the cell-free ingredients, which include designer genes that produce proteins only when triggered by certain strands of DNA or RNA, such as the RNA of the virus. The mixture was then placed on paper and freeze dried. When the Ebola RNA – from a saliva or blood sample – was added to the test paper, the genes produced proteins that turned the paper from yellow to purple. The paper detector is not yet ready for field tests. Collins wants to make it more sensitive so that smaller samples can be tested, and he wants to make sure it has a low false-positive rate. But he’s working fast. His team needed just 12 hours to create the first version of the test.
This article first appeared in the December 2014 First Look section of ASEE’s Prism magazine and was written by chief correspondent Thomas K. Grose.
Meanwhile, a team of Johns Hopkins University biomedical engineering faculty and students designed a more effective and comfortable protective suit for caretakers of Ebola patients. Their design beat out 1,500 other contenders in the U.S. Agency for International Development’s 2014/15 global design competition Fighting Ebola: A Grand Challenge for Development.
Team leader Youseph Yazdi, an assistant professor of biomedical engineering and executive director of the Johns Hopkins Center for Bioengineering Innovation and Design (CBID) said the team was engaging a major protective suit manufacturer to license its design and have product available by summer. “This Ebola outbreak killed over 10,000 people, many more than prior outbreaks. The world can’t afford to get caught flat-footed when the next infectious disease outbreak hits, and this new protective suit will help us be better prepared and protect the brave men and women at the front lines of the response,” Yazdi said.
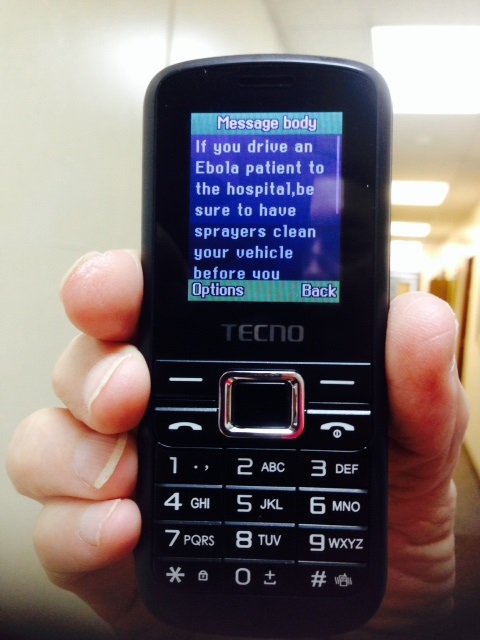
The Centers for Disease Control and Prevention’s Ebola efforts in Africa during 2014 including text messaging 1.5 million subscribers in Liberia, Sierra Leone, and Guinea. (Photo, right)
Don’t expect fast miracles, however. As Prism‘s February 2018 cover story noted, biotechnology has a sluggish track record of moving products from lab to profitable market (“Slow to Bite“).
Consider Intrexon, a biotech firm that has developed apples that won’t turn brown when sliced, salmon raised in tanks on land in half the time it takes the ocean variety to grow, and a variety of medical innovations, including a cloned toy poodle named Baxter. The company also has been working on a genetically modified mosquito engineered to suppress the Aedes aegypti mosquito, which spreads the Zika and dengue viruses. The technique modifies male Aedes mosquitoes, which don’t bite, to produce offspring with a “self-limiting” gene that causes them to die before reaching adulthood.
The trademarked Friendly™ mosquito was developed by an Oxford University spinoff, Oxitec Ltd., that Intrexon acquired in 2015. It was one of several bioengineered mosquitoes that the U.S. Environmental Protection Agency approved for a test release in 20 states in 2017. In 2019, a study suggesting that the genetically modified mosquito may be making its virus-transmitting brethren more potent, not less, sparked a backlash.
Filed under: Special Features
Tags: Biomedical Engineering, CDC, disease diagnosis, ebola, genetically modified mosquitoes, Gottingen University, Harvard Wyss Institute, Intrexon, paper-based diagnostic test, suitcase lab, Zika